- Home
- Live Blog
- Breaking News
- Top Headlines
- Cities
- NE News
- Sentinel Media
- Sports
- Education
- Jobs
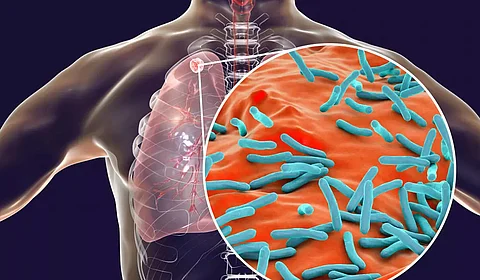
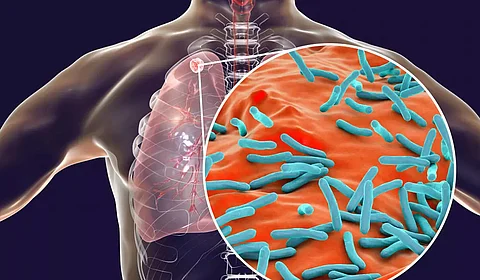
India’s tuberculosis (TB) case notification in 2022 increased to a record 24.22 lakh in 2022, surpassing the pre-COVID level of 24 lakh in 2019. While this signifies that the country is overcoming the challenges posed by pandemic disruption, the target set by the Central Government to make India TB-free under the National TB Elimination Programme (NTEP) by 2025 remains a daunting task. The Parliamentary Standing Committee on Health and Family Welfare points out that, keeping in view the challenging situation to curb the rise in new TB cases, especially the complex drug-resistant TB cases, the “task at hand is enormous and is short” to meet the target. The data presented in the “India TB Report 2023” speaks volumes about the ground realities. The year 2022 saw an increase of 32% in the number of multidrug-resistant/refampicin (MDR/RR-TB) cases detected under NTEP as compared to 2021, it states. Among the five risk factors that together account for 44% of TB incidence in the country are undernutrition, harmful use of alcohol, smoking, and HIV. Therefore, the convergence of health interventions to address these risk factors under various flagship programmemes can significantly contribute towards the TB elimination programme. The objectives of providing TB treatment services under NTEP include rapidly making the patient non-infectious, breaking the chain of transmission, and decreasing the probability of transmission of TB infection; decreasing case fatality and morbidity by ensuring a relapse-free cure; and minimising and preventing the development of drug resistance. A worrying finding from the National TB Prevalence Survey highlighted in the TB report is that 64% of TB-symptomatic individuals did not seek treatment. The most common reason (68%) cited is ignoring the symptom; 18% did not recognise the symptoms of TB; 12% cited the reason of self-treatment; and 2% said they were unable to afford the care. The figures are reflective of the yawning gap in the TB prevention and elimination campaign and the accessibility of TB treatment and care, not reaching out to a wider section of the population. The parliamentary panel has taken note of this gap and recommended that there is a requirement for systematic planning and implementation of active case-finding campaigns among vulnerable populations in community settings more aggressively so as to minimise the delays in the detection and treatment of TB cases. The Central Government’s response to address this gap led to the articulation of the Pradhan Mantri TB Mukt Bharat Abhiyan (PMTBMBA), which was launched on September 9 last year. Prime Minister Shri Narendra Modi, in one of his Mann Ki Baat epidoes, laid emphasis on “Jan Bhagidari” (people’s participation) at scale to accelerate ending TB in India and said, “I believe that with this power of public participation, India will definitely be free from TB by the year 2025.” The World Health Organisation (WHO), in its report titled ‘Implementing the End TB Strategy: The Essentials’, released in 2022, harps on three pillars of intervention: ‘Integrated patient-centred care and prevention’, which puts people living with TB at the heart of service delivery; ‘Bold policies and supportive systems’ that require intense participation across government, communities, and private stakeholders; and the third pillar is ‘Intensified research and innovation’, which the global health body says is critical to breaking the trajectory of the TB epidemic and reaching global targets. The parliamentary panel notes that PMTBMBA to end TB in India is aligned to these three pillars and suggests putting in place a robust mechanism selection and monitoring for the new Community Connect Initiative under the mission known as Ni-kshay Mitra Initiative. The initiative is aimed at approaching all active TB patients to obtain their consent for receiving community support from the donors referred to as Ni-kshay Mitra. Official statistics show that as of April 27, more than 79,000 Nikshay Mitras have come forward to support more than 9 lakh TB patients, and over 5.47 lakh food baskets have been distributed across the country. The critical view of the parliamentary panel is that the Ni-kshay adoption model cannot be considered the mainstay of fighting against TB and achieving the target of eradicating TB by 2025. The Committee further expresses its concerns about the “oversense of complacency within the Ministry and the government organisation” responsible for implementing the TB elimination programme due to the shift in their responsibility to non-governmental organisations, which, it cautions, “eventually may impede the overall progress”. Such timely observation and caution by the committee is expected to be taken note of by the government for undertaking necessary course correction so that ending TB by 2025 does not remain a mere slogan but all stops in the pathway are pulled out in time. Another key recommendation made by the parliamentary committee that warrants active consideration by the Central Government is decentralisation of funds, so the states are better equipped to address their region-specific challenges and need-based requirements for TB eradication.