- Home
- Live Blog
- Breaking News
- Top Headlines
- Cities
- NE News
- Sentinel Media
- Sports
- Education
- Jobs
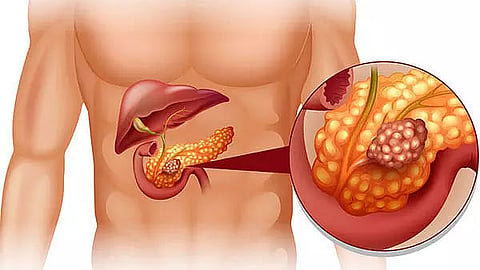
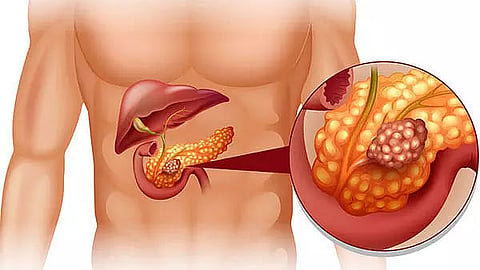
Acute pancreatitis is a medical condition characterized by the inflammation of the pancreas, a vital organ located behind the stomach. The pancreas plays a crucial role in digestion by secreting enzymes and hormones, including insulin. When the pancreas becomes inflamed, it can cause severe discomfort and lead to multiple complications affecting different organs, including the lungs, kidneys, and digestive system.
The symptoms of acute pancreatitis can be sudden and severe, often requiring immediate medical attention. These include:
Severe pain in the upper abdominal region
Pain radiating towards the back
Fever
Rapid heart rate
Nausea and vomiting
Tenderness in the abdominal area
In the case of chronic pancreatitis, the symptoms may be more prolonged and include:
Persistent upper abdominal pain
Pain worsening after meals
Unexplained weight loss
Greasy and foul-smelling stools
Pancreatitis occurs when digestive enzymes become active while still inside the pancreas, leading to irritation and inflammation of pancreatic cells. Several factors can trigger this condition, including:
Excessive alcohol consumption
Certain medications
Gallstones
High levels of triglycerides in the blood
Pancreatic cancer
Bacterial or viral infections
Abdominal injuries
Obesity
Some risk factors increase the likelihood of developing pancreatitis, such as:
Heavy alcohol use
Cigarette smoking
Diabetes
Family history of pancreatitis
Pancreatitis can result in several severe complications, including:
Acute pancreatitis can impact lung function, leading to difficulty in breathing. The inflammation of the pancreas reduces oxygen levels in the body, which can cause respiratory distress and oxygen deprivation.
Debris and fluids may accumulate inside the pancreas, forming pockets that resemble cysts. These pseudocysts can cause additional complications such as infections or internal bleeding.
In severe cases, pancreatitis can impair kidney function, potentially requiring dialysis.
Pancreatitis affects the secretion of digestive enzymes, leading to poor digestion and sudden weight loss.
Inflammation of the pancreas may damage insulin-producing cells, increasing the risk of diabetes.
Several diagnostic tests and procedures can confirm pancreatitis, including:
Blood tests: To check for elevated pancreatic enzymes and assess kidney function.
Ultrasound: To detect gallstones and signs of pancreatic inflammation.
CT Scan: To evaluate the severity of inflammation and identify potential complications.
MRI: To detect abnormalities in the pancreas and bile ducts.
Endoscopic ultrasound: To assess blockages or inflammation in the pancreatic duct.
Stool test: To determine the level of undigested fats in the body.
Treatment for acute pancreatitis typically involves:
Early Eating: Once symptoms improve, patients are encouraged to resume eating. Starting with clear liquids and soft foods can help the pancreas recover.
Pain Management: Pain relievers may be prescribed to ease discomfort.
Intravenous Fluids (IV Fluids): Administered through veins to support hydration and promote healing.
Nutritional Support: In severe cases, a feeding tube may be required if a patient cannot tolerate solid foods.
Once the inflammation is under control, doctors may recommend additional treatments:
Endoscopic retrograde cholangiopancreatography (ERCP): A procedure used to remove obstructions in the pancreatic or bile ducts.
Gallbladder Surgery: If gallstones cause pancreatitis, gallbladder removal may be necessary.
Pancreatic Procedures: Draining pancreatic fluid or removing diseased tissue if needed.
Alcohol Rehabilitation Programs: If alcohol consumption contributes to pancreatitis, lifestyle changes or rehabilitation may be required.
Medication Adjustments: If a specific medication is responsible for pancreatitis, the doctor may switch to an alternative.
For individuals suffering from chronic pancreatitis, long-term management includes:
Pain Management:
Prescribed pain relievers
Nerve block injections to prevent pain signals from reaching the brain
Digestive Enzyme Supplements:
Enzyme replacement therapy helps the body digest food properly.
Dietary Modifications:
A well-balanced diet with low-fat foods is essential.
Consultation with a dietitian may be recommended.
Pancreatitis is a serious condition that requires prompt medical intervention. Early diagnosis and treatment can prevent complications such as breathing difficulties, kidney failure, and malnutrition. Lifestyle modifications, including a healthy diet, quitting smoking, and limiting alcohol intake, can help manage and prevent pancreatitis. If you experience symptoms of pancreatitis, seek medical attention immediately to ensure proper treatment and recovery.
Also Read: Importance of Potassium
Also Watch: